By Amiri Wabusimba.
Uganda’s public health system has been caught in a cycle of crisis management for decades.
The country has been plagued by recurring outbreaks of deadly diseases like Ebola, Mpox, and Marburg.
Yet, despite the urgency and devastation these health emergencies cause, Uganda’s response continues to rely on short-term, reactive measures scrambling for emergency funds, seeking foreign aid, and implementing temporary containment strategies.
The lessons from previous outbreaks seem to fade with each decline in infection rates, only to resurface when the next crisis inevitably strikes.
In fact, Uganda has faced more than 10 Ebola outbreaks in the past 50 years with the most recent one, in January 2025, resulted in one death.
This cycle of crisis, response, and relapse underscores a fundamental flaw in Uganda’s approach to health.
Despite significant external support from USAID, UNICEF, and the Global Fund, Uganda remains dangerously dependent on foreign aid, a dependency that leaves the nation vulnerable to shifting priorities on the global stage.
The recent suspension of USAID funding should serve as a stark warning Uganda stands at a critical juncture. Either the country takes bold steps toward a self-sustaining health system, or it continues to rely on external aid, which often fluctuates based on political and economic shifts far beyond its control.
At the heart of Uganda’s public health crisis lies a glaring contradiction of government’s expenditure on administrative activities continue to rise, yet the health sector remains chronically underfunded.
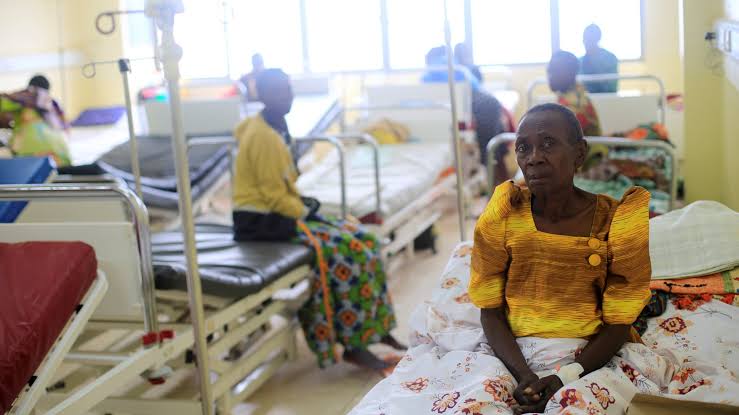
Public hospitals are routinely faced with shortages of medical supplies, while taxes collected from citizens are funneled into administrative luxuries rather than life-saving interventions.
The irony is undeniable a healthy population is the backbone of economic productivity, yet those tasked with managing the nation’s resources seem to ignore this reality.
For example, in the 2022-2023 national budget, Uganda allocated only 7.7% of its total spending to the health sector, far below the 15% target set by the African Union’s Abuja Declaration.
Despite this, health spending often fails to reach critical areas like medical supplies, infrastructure, and personnel compensation. Consequently, Uganda’s citizens, who are directly impacted by health crises, continue to bear the brunt of poor health funding.
Beyond funding challenges, Uganda’s inability to provide essential services such as clean water exacerbates its public health woes.
Urban and rural areas have faced critical water shortages during the dry season, with some communities going without water for over a month.
In the context of battling infectious diseases like Ebola and Mpox, this water scarcity becomes a grave concern.
Hand hygiene is a basic and effective measure in preventing the spread of these diseases, yet it becomes impossible to enforce when there is no water for handwashing.
According to a 2020 report by the World Health Organization, 38% of Ugandans lack access to basic water services, contributing to an environment ripe for the spread of diseases.
Without consistent access to water, Uganda cannot effectively control the transmission of disease, making it impossible to protect citizens from future outbreaks.
The solution lies not in waiting for the next foreign grant but in building a self-sustaining, community-driven health system.
One promising avenue is the establishment of a Community Health Insurance Scheme (CHIS), which could provide financial protection to Ugandans and strengthen health facilities from within.
A well-structured CHIS, similar to Rwanda’s Mutuelles de Santé model, could enable individuals to contribute small, regular payments that create a collective pool of resources to guarantee access to medical care without the financial burden of out-of-pocket expenses.
Rwanda’s success in implementing this model covering over 90% of its population proves that it is not only feasible but also effective.
For such a system to work in Uganda, however, Transparency in health financing is non-negotiable. Ugandans will not invest in a national health insurance model if they believe that funds will be mismanaged.
The government must demonstrate its commitment to health by passing the necessary legislation, ensuring public hospitals are equipped, paying health workers fairly, and maintaining a consistent supply of essential medicines.
While financial security is crucial, it alone will not prevent future outbreaks.
Prevention remains the most cost-effective approach to public health, and Uganda must prioritize integrated health campaigns that combine disease awareness, vaccination, maternal health education, and sanitation initiatives.
Rather than treating health issues in isolation, a comprehensive, community-centered approach should be adopted.
Uganda’s health messaging, too, must evolve to better resonate with local populations.
Health advisories in English often miss their mark with rural farmers who speak languages like Luganda or Runyankore.
Engaging religious and cultural leaders as trusted messengers and utilizing mobile technology to send health updates can enhance public awareness.
Community radio, an underutilized tool, can play a pivotal role in spreading health information, especially in rural areas.
Uganda’s health infrastructure must align with its ambitions of encouraging vaccination campaigns if rural clinics lack the basic infrastructure to store vaccines, or to promote handwashing if there is no access to water.
Uganda must invest in local health infrastructure, including better-trained health workers and improved disease surveillance systems, to respond rapidly to outbreaks before they escalate into national crises.
Innovations like mobile health technologies and telemedicine can bridge gaps, particularly in remote areas, providing vital health information and services where they are most needed.
Uganda cannot afford to continue functioning on borrowed time, waiting for the next international bailout to solve its health problems.
The country’s public health system must evolve from a reactive model to a proactive, self-sustaining one.
This requires increasing health funding, ensuring reliable water systems, prioritizing prevention, and developing a transparent, accountable healthcare system.
The time has come for Ugandans to take control of their own health future not as recipients of foreign aid, but as architects of sustainable solutions.
The health of a nation is directly tied to its economic productivity, and it is in Uganda’s best interest to invest in its people and their well-being.

Amiri Wabusimba is a diplomatic Scholar, Journalist, political analyst and Human Right activist. Tel: +56775103895 email: Wabusimbaa@gmail.com.
Have An Advert Or Article You Want Us To Publish? Whatsapp: +256786288379 or email binocularugnews@gmail.com